Spondylolisthesis
What is spondylolisthesis?
Spondylolisthesis occurs when one vertebra slips forward on the one below it, most often in the lower back. It can be degenerative (age-related), related to a small stress fracture (isthmic), or less commonly from injury.
What are the symptoms?
Lower back pain and leg pain (sciatica) are common. Some people notice numbness, weakness, or pain that worsens with standing or walking and improves with sitting.
How is it treated?
Non-surgically, spondylolisthesis can be treated with physical therapy, core strengthening, bracing and pain management methods. Injections can help. If symptoms persist, surgery may involve decompression to free the nerves, and fusion only when there is instability. In many adults with degenerative spondylolisthesis and stenosis, decompression alone can perform as well as decompression with fusion.
Sciatica
What is sciatica?
Sciatica refers to leg pain caused by irritation of a lower spine nerve root, usually L4, L5, or S1. The most common causes are a herniated disc or spinal narrowing.
What are the symptoms?
People typically experience sharp or burning pain down their leg along with numbness, tingling or weakness that usually worsens when sitting, coughing or with prolonged standing.
How is it treated?
Medications, physical therapy, and epidural steroid injections are the typical first treatments. The surgical treatment is a minimally invasive lumbar discectomy where we remove the disc fragment that is compressing the nerve root with minimal tissue disruption and a quick recovery.
Degenerative Disc Disease (DDD)
What is degenerative disc disease?
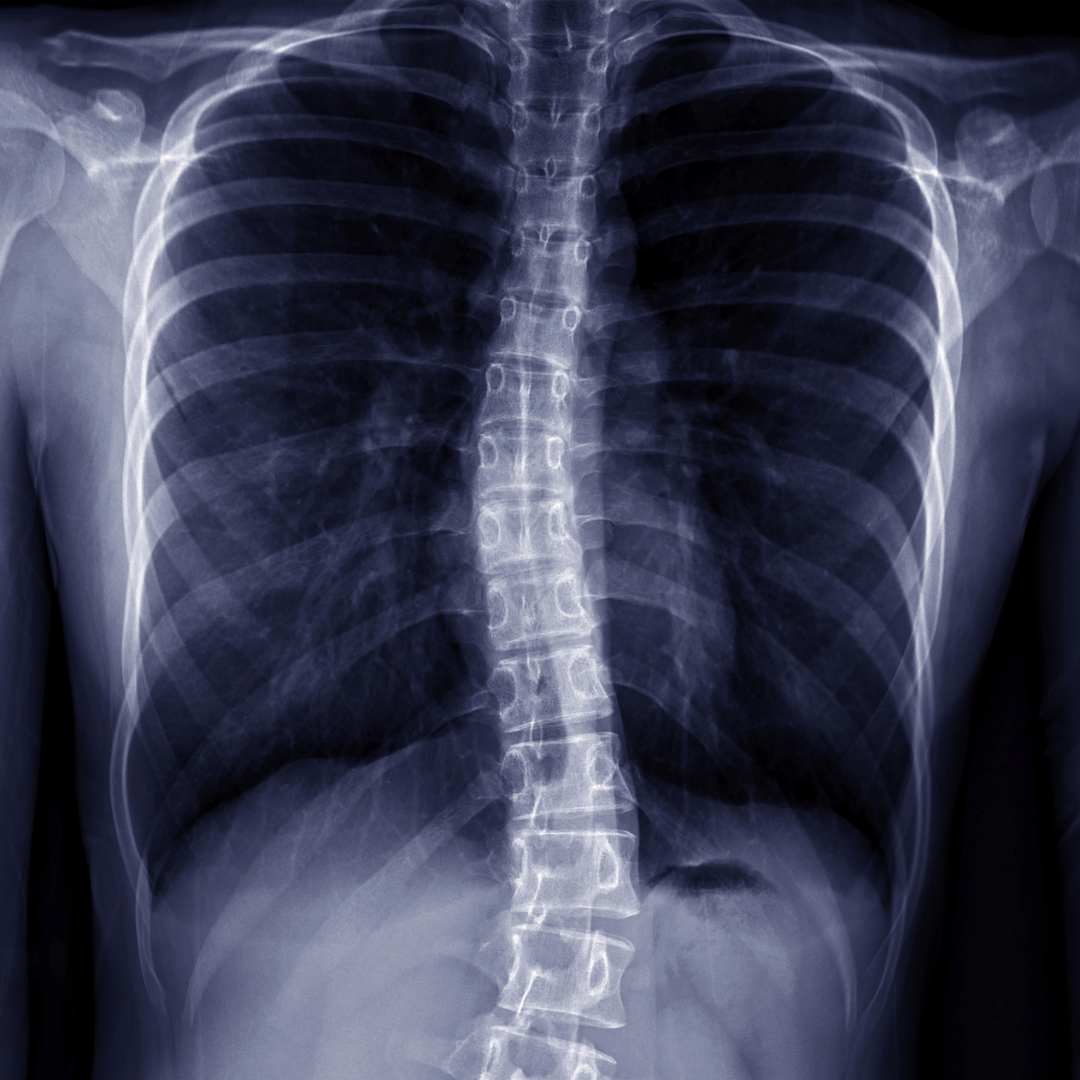
Despite the name, it is not a “disease.” It is age-related disc wear and dehydration that is common on x-rays or MRI.
What are the symptoms?
It can be painless, but when symptomatic it often causes stiffness, and achy neck or low back pain that worsens with sitting, bending, activity, or lifting.
How is it treated?
Non-surgical options include activity modification, physical therapy, medications, and injections. Injections especially be helpful during flares. Surgery is usually considered when we are also addressing a surgically treatable problem, most often nerve compression or spinal stenosis, where decompression, sometimes with fusion, is appropriate. In the cervical spine, options include motion-preserving disc replacement or ACDF (fusion) when symptoms and imaging align. In the lumbar spine, carefully selected patients with discogenic pain may be candidates for lumbar disc replacement after other sources of low back pain have been ruled out, and a full course of nonsurgical care is completed. A newer option for discogenic low back pain is basivertebral nerve ablation. In patients with the right MRI findings, studies show durable improvements in pain and function.
Pinched Nerve (Radiculopathy)
What is a pinched nerve?
Radiculopathy means a spinal nerve root is compressed or irritated, commonly by a herniated disc, bone spur, or spinal stenosis.
What are the symptoms?
People often experience radiating pain in their arms or legs, numbness or tingling, and/or muscle weakness along that nerve’s pathway.
How is it treated?
Start with anti-inflammatory medications, physical therapy, and targeted injections. For cervical radiculopathy, removing the disc from the front (anterior cervical discectomy) is typically followed by either fusion (ACDF) or cervical disc replacement. For lumbar radiculopathy from a disc herniation, a minimally invasive microdiscectomy is common when symptoms persist.
Herniated Disc
What is a herniated disc?
A herniated disc occurs when the inner gel of a spinal disc pushes through a tear in the outer wall and can press on a nearby nerve, most often in the lower back.
What are the symptoms?
People often experience sudden back or neck pain and may later develop radiating nerve pain (sciatica or arm pain), and numbness or weakness.
How is it treated?
Most people improve with time, activity modification, physical therapy, and medications. Injections can help reduce inflammation and sciatica pain. If significant pain or weakness persists, a minimally invasive discectomy can remove the disc fragment. In the neck, ACDF or disc replacement are options when indicated.
Bulging Disc
What is a bulging disc?
A bulging disc means the disc’s outer wall protrudes outward without a full thickness tear. Bulges are common and often asymptomatic, but they can cause back pain. Sciatica symptoms arise only if the bulge is large enough to narrow the space available for a nerve nearby.
What are the symptoms?
People often experience back, neck, or less commonly, radiating nerve pain, but their symptoms are typically milder than if they had a herniated disc.
How is it treated?
Bulging discs can be treated conservatively with physical therapy, medications, and posture correction. If clear nerve compression persists despite conservative care, a minimally invasive microdiscectomy in the lower back may be performed.